Knee Bursitis
Knee bursitis is inflammation of a small fluid-filled sac called a bursa that sits near your knee joint. Bursae reduce friction and cushion pressure points between your bones and the tendons, muscles and skin near your joints.
Any of the bursa in your knee can become inflamed, but knee bursitis most commonly occurs over the kneecap or on the inner side of your knee below the joint.
Knee bursitis causes pain and can limit your mobility. Treatment for knee bursitis often includes a combination of treatments you can do yourself and doctor-administered treatments to get rid of your pain and inflammation.
What are the symptoms of Knee Bursitis?
Knee bursitis signs and symptoms can vary, depending on which bursa is affected and what's causing the inflammation.
In general, the affected part of your knee might feel warm, tender and might be swollen particularly when you put pressure on it. You might also feel pain when you move or sometimes even when you are resting.
A sharp blow to the knee can cause symptoms to appear rapidly. But most cases of knee bursitis result from friction and irritation of the bursa that occurs in jobs that require a lot of kneeling on hard surfaces — so symptoms usually begin gradually and can worsen over time.
When should I see a doctor?
The bursa that lies over your kneecap can sometimes become infected. Call your doctor if you have a temperature in addition to worsening pain and swelling in your knee.

What causes Knee Bursitis?
Knee bursitis can be caused by:
- Frequent and sustained pressure, such as from kneeling, especially on hard surfaces
- Overuse or strenuous activity
- A direct blow to your knee
- Bacterial infection of the bursa
- Complications from osteoarthritis, rheumatoid arthritis or gout in your knee
Am I at risk of getting Knee Bursitis?
Knee bursitis is a common complaint, but your risk of developing this painful disorder can be higher from:
- Prolonged kneeling. People who work on their knees for long periods — carpet layers, plumbers and gardeners — are at increased risk of knee bursitis.
- Participation in certain sports. Sports that result in direct blows or frequent falls on the knee — such as rugby, football and volleyball — can increase your risk of knee bursitis. Runners can develop pain and inflammation in the pes anserine bursa, situated on the inner side of your knee below the joint.
- Obesity and osteoarthritis. Pes anserine bursitis, affecting the inner side of your knee below the joint, often occurs in obese women with osteoarthritis.
How can I Avoid Getting Knee Bursitis?
To avoid knee bursitis or prevent it from coming back you can try the following:
- Wear kneepads. If you're working on your knees or participating in sports that put your knees at risk, use padding to cushion and protect your knees.
- Take breaks. If you're on your knees for a period of time, take regular breaks to stretch your legs and rest your knees.
- Avoid excessive squatting. Excessive or repetitious bending of your knees increases the force on your knee joints.
- Achieve and maintain a healthy weight. This can help take pressure off your knee joints.
How do You Diagnose Knee Bursitis?
In my specialist knee clinic often make a diagnosis of knee bursitis with from your symptoms and a physical examination. I will usually:
- Compare the condition of both knees, particularly if only one is painful
- Gently press on areas of your knee to detect warmth, swelling and the source of pain
- Inspect the skin over the tender area for redness or other signs of infection
- Carefully move your legs and knees to determine your knee's range of motion and whether it hurts to bend or flex it
How do You Diagnose Knee Bursitis?
In my specialist knee clinic often make a diagnosis of knee bursitis with from your symptoms and a physical examination. I will usually:
- Compare the condition of both knees, particularly if only one is painful
- Gently press on areas of your knee to detect warmth, swelling and the source of pain
- Inspect the skin over the tender area for redness or other signs of infection
- Carefully move your legs and knees to determine your knee's range of motion and whether it hurts to bend or flex it
Do I need special tests to diagnose Knee Bursitis?
To help rule out injuries that can cause signs and symptoms similar to those of bursitis, I might sometimes request one or more of the following imaging tests:
- X-ray. These can be useful in revealing a problem with a bone or arthritis.
- MRI. MRIs use radio waves and a strong magnetic field to produce detailed images of structures within your body. This technology allows me to see soft tissues, such as bursae.
- Ultrasound. Using sound waves to produce images in real time, ultrasound can help us to visualise the swelling in your affected bursa.
How do you Treat Knee Bursitis?
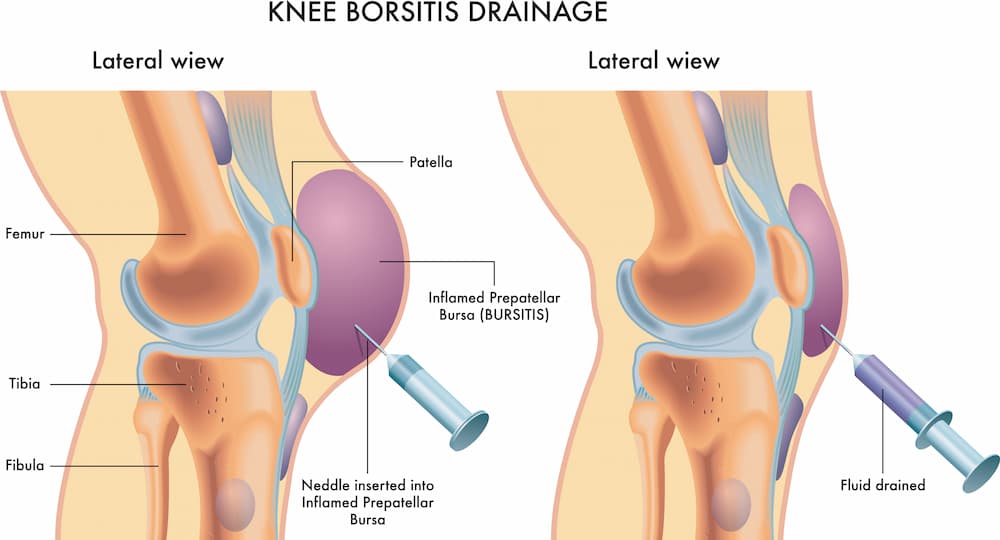
Aspiration
If I suspect that you have an infection or gout in the bursa, I might take a sample of the bursa fluid for testing by inserting a needle into the affected area and draining some of the fluid. This can also be used as treatment.
Bursitis often improves over time, so treatment is usually aimed at symptom relief. However, depending on the cause of your knee bursitis and which bursa is infected, I might recommend one or more treatment approaches.
Medications
If an infection has caused the knee bursitis, I will prescribe a course of antibiotic treatment.
Therapy
I might refer you to a physiotherapist or specialist in sports medicine, who can help you improve flexibility and strengthen muscles. This therapy might get rid of your pain and reduce your risk of recurring episodes of knee bursitis. Protective knee braces might help if you can't avoid kneeling, and compressive knee sleeves can help reduce swelling.
Surgery and other procedures
More-invasive treatments for knee bursitis treatment include:
- Corticosteroid injection. If the bursitis is persistent and not responding to basic treatments, I might consider injecting a corticosteroid drug into an affected bursa to reduce inflammation. The inflammation usually subsides rapidly, but you might have pain and swelling from the injection for a couple of days.
- Aspiration. I might aspirate a bursa to reduce excess fluid and treat inflammation. I will insert a needle into the affected bursa and draw fluid into the syringe. Aspiration might cause short-term pain and swelling, and you might need to wear a knee immobilizer for a short period after the injection to reduce the chance of recurrent swelling.
- Surgery. If you have severe chronic or recurrent bursitis and don't respond to other treatments, I might recommend surgery to remove the bursa.
More info
Read more about useful knee bursitis stretches and exercises.