Unravelling Osteoarthritis: Decoding its Genetic, Metabolic, and Chemical Dimensions
Osteoarthritis (OA) is a prevalent joint disorder affecting millions of people worldwide. It is a multifactorial condition that arises from a complex interplay of genetic, metabolic, and chemical factors. In this blog post, I’ll delve into the fascinating world of OA and explore how these aspects contribute to its development and progression.
Genetic Factors: Unravelling the Genetic Code of OA
Research has shown that genetics plays a pivotal role in the susceptibility to OA. While there isn't a single "OA gene," multiple genetic variations have been identified that contribute to an increased risk. Variants in genes encoding components of cartilage structure, extracellular matrix proteins, inflammatory mediators, and enzymes involved in cartilage metabolism have all been implicated.
Studies have demonstrated that certain genetic factors can affect the integrity of cartilage, leading to a decreased ability to repair damaged tissue. Moreover, they can influence the production and breakdown of important molecules, such as collagen and proteoglycans, which are crucial for maintaining cartilage health. Understanding these genetic underpinnings provides valuable insights into the disease's origins and potential therapeutic targets.
Metabolic Factors: Unmasking the Metabolic Secrets of OA
Metabolism refers to the biochemical processes that occur within our bodies to sustain life. Perturbations in metabolic pathways can contribute to the development of OA. Obesity, for instance, is a well-established risk factor for OA, particularly in weight-bearing joints such as the knees and hips. Excess weight places additional stress on the joints, accelerating wear and tear.
Metabolic syndrome, characterized by obesity, high blood pressure, abnormal lipid levels, and insulin resistance, is also associated with an increased risk of OA. Studies suggest that metabolic dysregulation can trigger chronic low-grade inflammation, oxidative stress, and altered lipid metabolism, all of which contribute to the progression of OA. Targeting metabolic abnormalities through lifestyle modifications and pharmacological interventions may help manage and prevent OA.

Chemical Factors: The Inflammatory Symphony of OA
Inflammatory cytokines, such as interleukin-1β (IL-1β) and tumor necrosis factor-alpha (TNF-α), play a critical role in the pathogenesis of osteoarthritis (OA). These signaling molecules are produced by various cell types, including immune cells, chondrocytes (cartilage cells), and synovial cells within the joint.
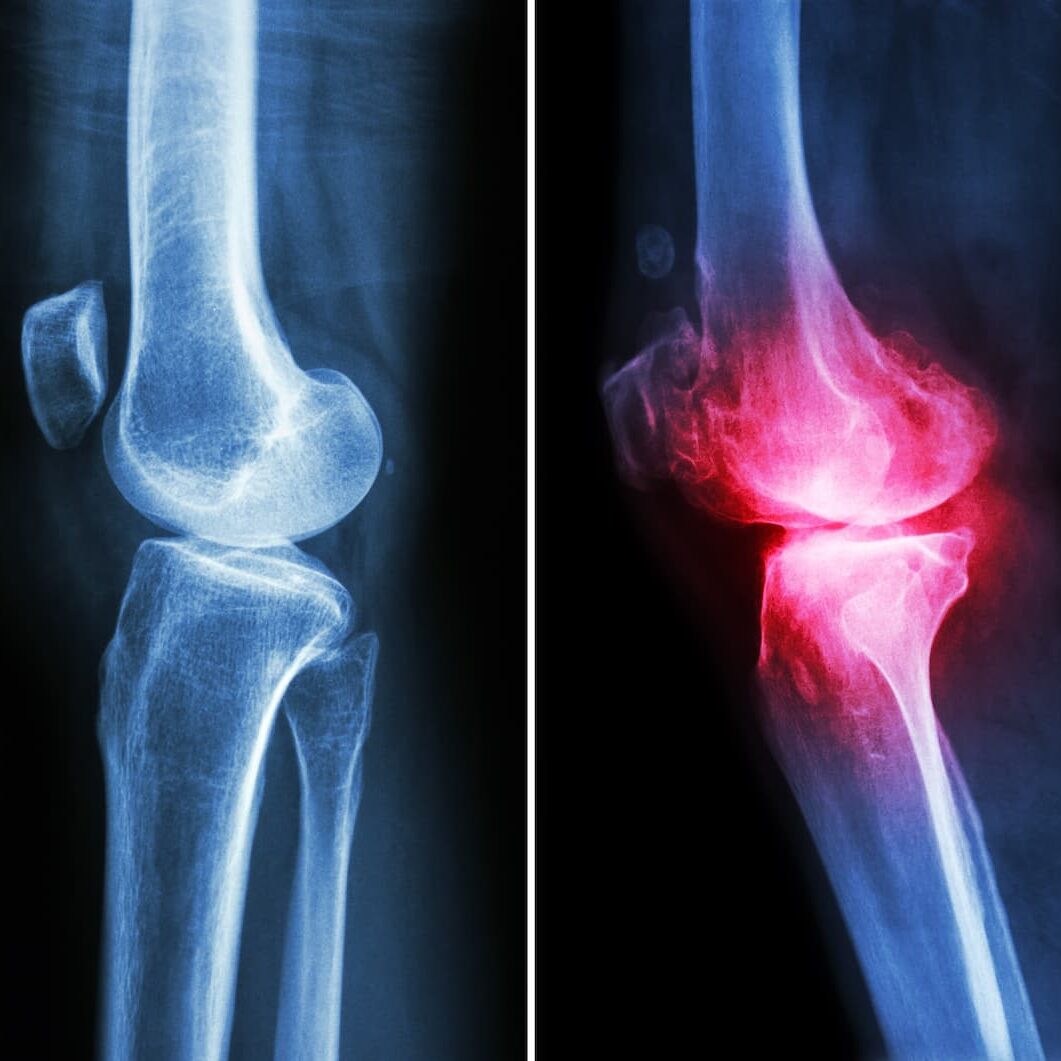
Cartilage Catastrophe: Inflammatory Cytokines and Cartilage Degradation in OA
IL-1β and TNF-α have a profound impact on cartilage health by promoting cartilage degradation. These cytokines stimulate the release of enzymes called matrix metalloproteinases (MMPs) from chondrocytes and synovial cells. MMPs are responsible for breaking down components of the extracellular matrix in cartilage, including collagen and proteoglycans. The excessive activity of MMPs leads to the destruction of the cartilage matrix, resulting in the characteristic loss of cartilage in OA.
Furthermore, IL-1β and TNF-α inhibit the synthesis of collagen and proteoglycans by chondrocytes. Collagen provides the structural framework for cartilage, while proteoglycans help retain water within the matrix, ensuring its elasticity and shock-absorbing properties. Reduced collagen and proteoglycan production compromises the integrity and function of the cartilage, contributing to its deterioration in OA.
Fuelling the Flames: Inflammatory Cytokines, Inflammation, and Pain in OA
Inflammatory cytokines also trigger and perpetuate the inflammatory response within the joint. IL-1β and TNF-α stimulate the production of other pro-inflammatory molecules, including additional cytokines, chemokines, and prostaglandins. These molecules attract immune cells to the joint, resulting in a chronic low-grade inflammation known as synovitis.
Synovitis further contributes to the progression of OA by releasing destructive enzymes and reactive oxygen species that harm the cartilage. The inflammation also leads to the thickening of the synovial membrane, causing pain, swelling, and stiffness in affected joints. Chronic pain in OA is partly a result of the inflammatory mediators sensitizing nerve endings and altering pain perception.
Feedback Loop of Doom: Inflammatory Cytokines and the Vicious Cycle of OA
IL-1β and TNF-α also stimulate the production of more IL-1β and TNF-α, creating a positive feedback loop. This perpetuates the inflammatory response, amplifying cartilage degradation and inflammation within the joint. The continuous presence of these cytokines disrupts the delicate balance between cartilage breakdown and repair, ultimately leading to the progressive loss of cartilage in OA.

Fighting Fire with Precision: Targeting Inflammatory Cytokines in OA Treatment
Understanding the role of inflammatory cytokines in OA has paved the way for the development of therapeutic strategies aimed at modulating their activity. Researchers have explored various approaches, including:
1. Cytokine Inhibitors: Biologic drugs that specifically block IL-1β or TNF-α have shown promise in reducing inflammation and slowing cartilage degradation in OA. These inhibitors work by binding to the cytokines, preventing them from binding to their receptors and exerting their destructive effects.
2. Anti-Inflammatory Agents: Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are commonly used to manage pain and inflammation in OA. They act by suppressing the production or activity of inflammatory mediators, including cytokines, providing symptomatic relief.
3. Disease-Modifying Osteoarthritis Drugs (DMOADs): DMOADs are a class of drugs being developed to modify the underlying disease processes in OA. Some DMOADs target inflammatory cytokines directly, while others aim to modulate the cellular pathways involved in cartilage breakdown and repair.
By targeting inflammatory cytokines and their downstream effects, these therapeutic interventions hold the potential to slow disease progression, alleviate symptoms, and improve the quality of life for individuals with OA.
Cracking the Code: Understanding the Genetic, Metabolic, and Chemical Dimensions of Osteoarthritis for a Promising Future
Osteoarthritis is a multifaceted condition influenced by genetic, metabolic, and chemical factors. Genetic variations can affect cartilage integrity and the production of key molecules, while metabolic factors like obesity and metabolic syndrome contribute to joint stress and inflammation. Chemical factors, including occupational hazards and smoking, can further exacerbate joint damage. By comprehensively understanding the genetic, metabolic, and chemical aspects of OA, researchers are paving the way for novel treatment strategies and preventive interventions. Continued research and advancements in these areas hold the promise of a brighter future for individuals affected by osteoarthritis.